Two St Catharine’s Fellows are part of a team of scientists and doctors that showed for the first time that a new assessment tool holds major promise for diagnosing and monitoring large vessel vasculitis (LVV), a group of diseases that affect the body’s blood vessels.
LVV is rare but causes chronic inflammation of the larger vessels that transport blood around the body, including the aorta and arterial branches leading on from it. Improving the diagnosis of LVV is crucial: early diagnosis and prompt treatment are associated with better quality of life and longer life expectancy for patients.
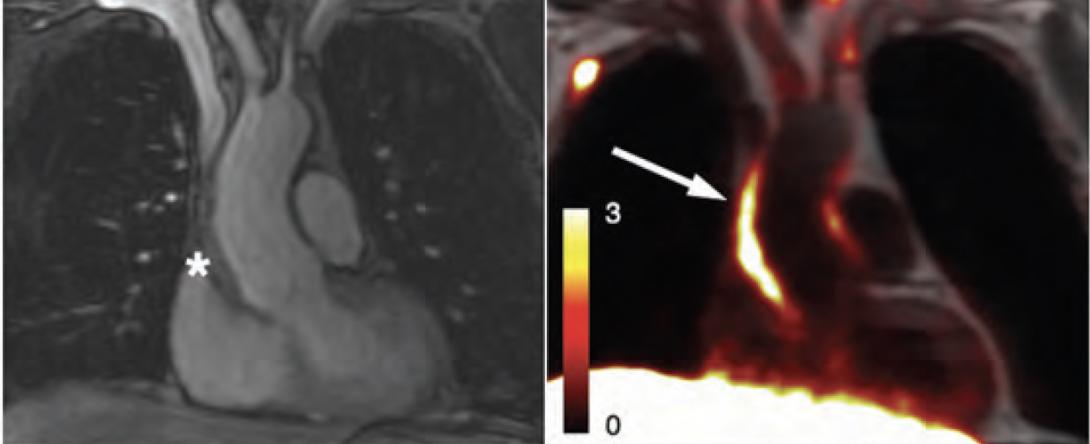
Dr Jason Tarkin (2021), Junior Research Fellow at St Catharine’s, and Professor Anthony Davenport (1995), Director of Studies in Preclinical Medicine and Pharmacology at St Catharine’s, worked with researchers across the UK to investigate whether repurposing an existing hospital imaging test – using a combined positron emission tomography (PET) and magnetic resonance imaging (MRI) scanner – could enable them to detect and monitor LVV by focusing on the expression of somatostatin receptor 2 (SST2).
SST2 is a protein that occurs naturally in the body and is found in the white blood cells (known as macrophages) responsible for the inflammation of blood vessels associated with LVV.
The research team trialled their new approach at Cambridge University Hospitals National Health Service Trust and Imperial College Healthcare National Health Service Trust with a group of patients who had active or inactive LVV. Results from their study showed that SST2-based imaging methods offer an accurate way to diagnose and monitor disease activity in people with LVV – and could also show the effectiveness of medicines prescribed to treat LVV.
Dr Tarkin, senior author of the study and Wellcome Clinical Research Career Development Fellow and Honorary Consultant Cardiologist at the University of Cambridge, commented:
“There is a real clinical need for better methods than are currently available for detecting arterial inflammation in patients with LVV. Our research showed for the first time that imaging SST2 in vessels could offer a novel method for diagnosing and monitoring LVV. The next step will be to test this new method in a larger head-to-head trial against the current standard PET imaging tracer, called FDG.”
Professor Davenport, co-author of the study and Professor of Cardiovascular Pharmacology at the University of Cambridge, said:
“This research is exciting because imaging allows clinicians to see what is happening inside the patient’s body before treatment and whether new medicines are effective in slowing the progression of LVV.”
Dr Tarkin added:
“I would like to express my gratitude to the large multidisciplinary study team, including Dr Andrej Ćorović, Dr Christopher Wall, Dr Meritxell Nus, Dr Helle Jørgensen and Professor James Rudd, among others. Above all, I would like to acknowledge the contributions of Professor Justin Mason, an inspirational mentor and leader in the field, who tragically passed away last year.”
This research was supported by funding from the Wellcome Trust, the British Heart Foundation and the NIHR Imperial Biomedical Research Centre.
Reference
Ćorović A, et al. Somatostatin Receptor PET/MR Imaging of Inflammation in Patients With Large Vessel Vasculitis and Atherosclerosis. Journal of the American College of Cardiology 2023; 81 (4). Available online at https://doi.org/10.1016/j.jacc.2022.10.034